RTDs are used to notify providers when there is something missing on the form or alert providers that there is questionable information on the claim. Timeliness for returning the completed RTD to Medi-Cal is within 60 days from the date the claim was received. The due date is specified at the top of the RTD.
Providers have two options when they receive an RTD:
Complete and return Part B (the bottom portion of the RTD). Submit a new claim, if timeliness permits. The RTD should be mailed in a plain business envelope to the following address:
HP Enterprise Services
P.O. Box 15200
Sacramento, CA 95851-1200
Medi-Cal receives the RTD, an operator keys in the corrections and the claim continues in the processing cycle.
Tip: Corrected information on the RTD must be in the same alphabetic or numeric format required on the claim form.
Note: The RTD must include an original signature of the provider or an authorized representative.
Section A – is to be retained by providers with a copy of the original claim.
Section B – is to be completed with corrections and returned by the date specified on the top portion of the RTD.
Rollover the highlighted fields with your mouse to learn about RTD form completion
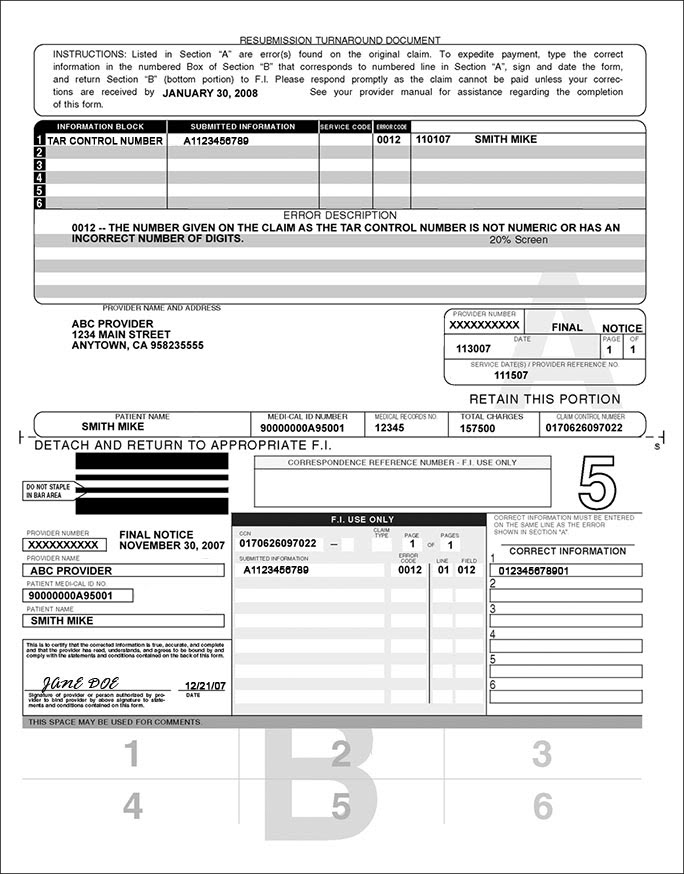
The top of the form (Portion A) contains instructions on how to complete the RTD and date the RTD must be returned to EDS, an HP company, with corrections.
If the information in Section A is correct, leave the corresponding line blank in Section B.
Purpose:
Eligibility Status Turn‐Around Documents (ESTD) are reports that are generated and sent to Income Maintenance (IM) Workers that detail a member’s spenddown eligibility and spenddown dollar amount.
These reports can be updated by the worker and returned to the Core unit to make updates in the Medically Needy sub‐system in the Medicaid Management Information System (MMIS).
Identification of Roles:
Adjustment Examiner – Processes returned/updated ESTD documents
Operations Coordinator ‐ Serves as a back‐up for processing ESTD documents
Operations Team Lead and Operations Manager – Monitors workload and ensures that work in completed in a timely manner
Performance Standards:
None
Path of Business Procedure:
Step 1: ESTD document is received via mail, email, or fax in OnBase from an Income Maintenance Worker
Step 2: Open file 17 in MMIS (Medically Needy Sub‐System)
Step 3: Determine what type of change will be made
a. Changing spenddown dollar amount
b. Eligibility changes
Step 4: Make changes in MMIS file 17 as requested by the IM Worker on the ESTD
a. If spenddown was already met and the IM worker requested changes, the ESTD should be returned to the IM Worker. The IM Worker letter should be completed in OnBase.
Step 5: Determine if adjustments are needed or if a claim needs resubmitted
a. Adjustments will be made if changes are made to an expense amount
b. Claims that have denied due to spenddown should be resubmitted, for the dates that were updated in file 17 of MMIS
c. If adjustments are needed to pharmacy claims an email should be sent to the Point of Sale (POS) unit.
1. Include the National Provider Identifier (NPI)
2. Member ID
3. Dates of Service
4. National Drug Code (NDC)
5. Spenddown dollar amount
Step 6: Complete the document in OnBase
a. Enter keyword information for the document
1. State ID is the only required keyword

